Upgrade your old RCM with the Next-Gen Elixir Billing, built on Salesforce to increase profitability
 Change is the only constant. With the ever-evolving healthcare landscape, new diseases coming up, new procedures are introduced, insurance clauses are changing due to uncertainty- as a healthcare provider you cannot afford to have an RCM that is of the past and takes so much time and money to adapt to new changes. What you need is an agile, robust and highly configurable open system which can adapt to any changes without flaws.
Change is the only constant. With the ever-evolving healthcare landscape, new diseases coming up, new procedures are introduced, insurance clauses are changing due to uncertainty- as a healthcare provider you cannot afford to have an RCM that is of the past and takes so much time and money to adapt to new changes. What you need is an agile, robust and highly configurable open system which can adapt to any changes without flaws.
Elixir is a one of a kind, Billing system which is built on Salesforce, specifically to mitigate errors, shorten revenue cycle and increase profitability. This article will mostly talk about the common problems in medical billing and how Elixir solves it all with less or almost no human intervention, saving time and money.
Most common problems of Medical Billers

1. Outdated patient insurance details in the system resulting in rejection or denials.
2. Revealing the cost of care only after the care is given, resulting in surprises and bad debts for patients and practices losing revenue after the care is given.
3. Manual claim generation resulting in data entry errors.
4. Missing out on procedures for claim generation, resulting in denials due to late submission of claims.
5. Various practices across states, with different contracted prices need to be incorporated into the billing.
6. Staffs are not reminded about anomalies at the right time resulting in loss of revenue.
7. Discrepancies in ERA is overlooked by staffs when dealing with huge volume of claims.
8. CXOs are unable to get the right reports and are not prompted of any threats well in advance.
These are not the only problems that Elixir focuses on, if you find this relevant, then book a free demo with us to know more.
The End-to-End Billing Solution by Elixir
Our customers love Elixir’s Solutions, let’s take a sneak peek into the benefits of it.
Automated Verification of Benefits
Many Billing systems may not have verification of benefits, even if they do, it needs to be checked manually. It gets super cumbersome to have it checked every now and then for all the patients that come to the facility.
Imagine a solution, which regularly checks your patients’ insurance details and their validity of benefit plans and much more and stores the most recent record in the system. Not just that, it alerts the staff members if your patients’ plans are going to get ended soon.
Pretty cool right? It takes the headache right off!
Cost of Care Calculation with a touch of Machine learning
In an ideal world, you go to a grocery store, pick an item, you see what the price is, and you know what you’re getting into. But when it comes to healthcare cost, it becomes a little grey as the cost depends on various factors from your insurance plan. To avoid any surprises both for the patients and providers, after the care is given, Elixir gives you the freedom to calculate a near to accurate cost upfront, not just by the insurance plans but based on our predictive analysis as well! All in the click of a button.
Now reduce surprises and get paid for sure.
The curious case of contracted prices
If you are a large practice, having various practices across the United States, then you probably would be having various contracted prices for the same procedure in different places. Now how do we accurately bill based on these? We cannot implement different software for each practice. But should we?
This is where the Salesforce’s out of the box handling of price books come into play. By adapting Elixir Billing, you get to implement a single unified software, all in the cloud, which seamlessly takes care of contracted prices for the same procedures and have it updated. So you don’t have to worry about entering and cross checking your prices. Simple, yet effective.
Automated Claim Generation
When a care is given, no procedure is going to get unattended for more than a day, because Elixir is cognitive of the procedures, it classifies the procedures as billable and non-billable automatically. Elixir generates claims for all the unattended procedures automatically in a periodic fashion and prompts the staffs for review before submission.
There is a minimum of 100 fields to be filled in a typical CMS 1500 form. Each form is going to take a minimum of 10-15 minutes if filled manually. Imagine a system which can generate all these forms for hundreds of patients in a single instance. Without Errors!
That’s how easy your lives are going to be with Elixir Billing.
Submitted a claim, why wait till ERA?
Claim processing is the one thing that is not in the providers control. Or is it?
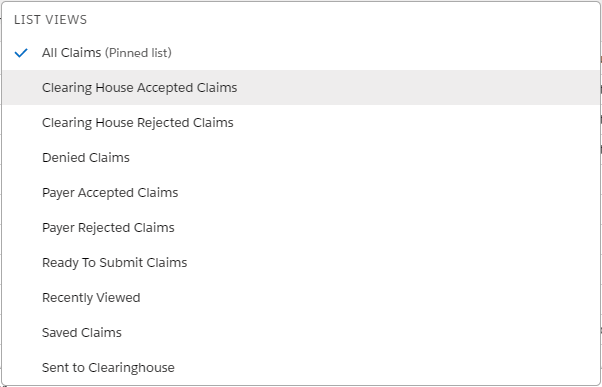
With Elixir, after submitting a claim as a provider, you are going to be aware of each level of statuses. Not just that, your staffs are going to be alerted about all the claims that are in the same status for more than few days, so that they can be tracked and accelerate the revenue cycle. This way you will always be in control of your claims.
In case, if a claim is rejected by the clearinghouse or payer for incorrect data, Elixir is intelligent enough to present only the incorrect fields and lets the staffs resubmit or does it automatically when it’s done.
Automatic ERA payment posting
For all the claims for which the ERA is back, Elixir will have the ERA data for each claim, on a procedure level, parsed, stored and reconciled. All it takes for the billing staff is to review it and post.
Usually, the staffs should go through thousands of ERA data and figure out for denials or underpayment. This is going to suck up all the precious time and increase the period of revenue cycle. Not with Elixir.
Elixir’s intelligent system, will store the data from ERA, be aware of any edge cases such as denied, underpaid and overpaid, by comparing the allowed amounts, and puts these claims in specific queues automatically. Not just that, the staffs are reminded about these queues on a regular basis.
If provider wants to resubmit these denied claims, the system will suggest the appropriate resubmission codes based on the adjustment codes that were sent.
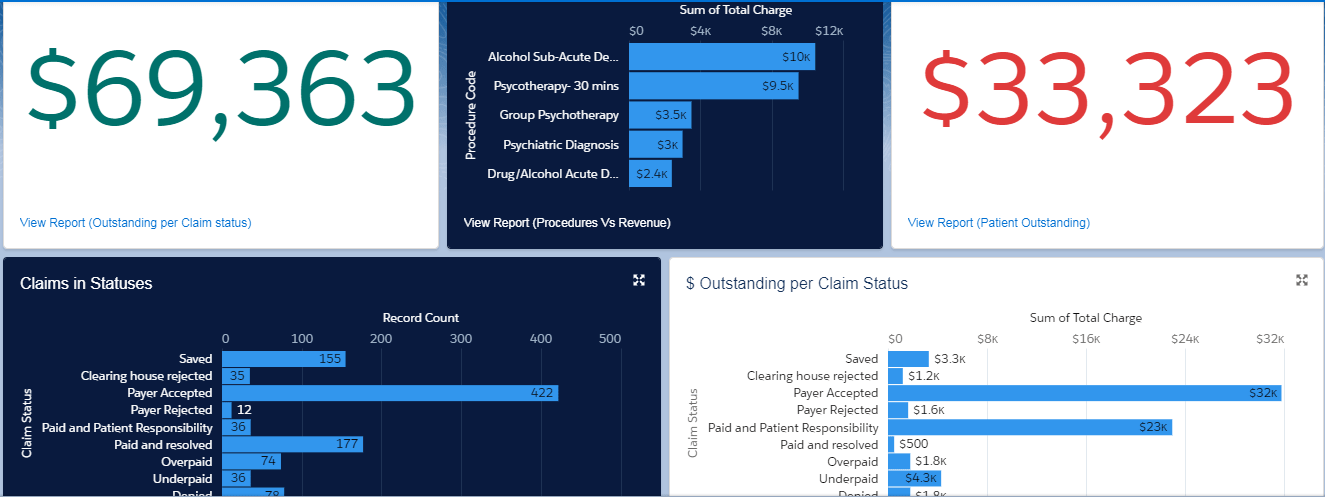
Stunning Data Visualizations, Relevant Reports, Predictive Analytics
Being built on Salesforce, every field in the system can be used for reporting. As a CXO of your hospital, you can get precise information about the past and the future of your Revenue cycle in the most stunning manner with out of the box reports and dashboards. Elixir uses Salesforce Einstein for data processing and analytics, giving you one of the most proven analytic tools in the world.
Step into the world of better healthcare Billing
Elixir Billing focusses on Mitigating errors, ease of use, shorten the revenue cycle time and accelerate profitability. Upgrade your medical billing software today and step into the future with Elixir and get the power of world’s best CRM Salesforce working towards increasing your practice profitability.
Take a test drive at https://www.elixirehr.com/take-a-test-drive/, to increase your healthcare facility’s profitability.


